Your Lack of Sleep Is Hurting You
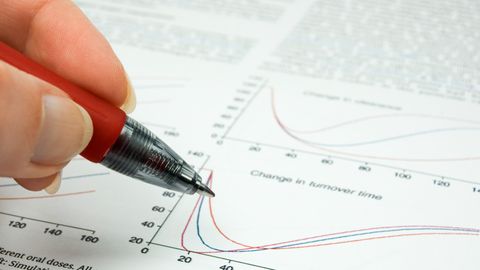
The mechanism by which sleep disruption can lead to heightened pain sensitivity has been investigated

Complete the form below to unlock access to ALL audio articles.
Around 1.5 billion people suffer from chronic pain worldwide, which has been linked to a range of comorbidities, including sleep disorders. A multi-institutional study led by Dr. Shiqian Shen at Massachusetts General Hospital and published in Nature Communications, demonstrated the mechanism by which sleep disruption can lead to heightened pain sensitivity and therefore a greater perception of pain.
Chronic sleep disruption and pain sensitivity
Research has shown that chronic sleep disruption (CSD) promotes pain, also known as hyperalgesia, which can commonly be experienced as headaches or body pain after a night of poor sleep. However, the mechanisms underlying this phenomenon have been relatively unexplored. For people with sleep disorders, CSD can result in heightened pain perception on a regular basis, which can impede daily activities and routine, thereby indicating the importance of gaining a better understanding of the neural underpinnings that cause hyperalgesia in people experiencing sleep disruptions. Dr. Shen’s team hypothesized that the thalamic reticular nucleus (TRN), which has been implicated in arousal and sleep spindle generation, may be involved in CSD-induced hyperalgesia.
The role of the TRN, VP and NADA in CSD-induced hyperalgesia
The researchers worked under a validated paradigm to induce sleep deprivation in C57/BL6 mice for five consecutive days. Group sizes for different parts of the experiment ranged from 3 to 16 mice. They used metabolomics to analyze the presence of metabolites in different brain regions associated with the TRN using LC-MS/MS techniques to improve understanding of the metabolic changes associated with sleep disruption. In order to test for pain sensitivity, the researchers measured the mechanical and thermal withdrawal thresholds of the mice in response to specific stimuli, including heat. They also used fiber photometry to study calcium signals associated with neural activity, and they used viral vectors and optogenetics to selectively inhibit neurons.
The key findings from the study were that:
- Inhibiting TRN neurons led to decreased withdrawal thresholds, indicating an onset of hyperalgesia, whereas activating TRN neurons reduced CSD-induced hyperalgesia.
- Mice with CSD experienced greater pain sensitivity after chemogenetic inhibition of neurons in the ventrobasal complex of the thalamus (VP) that received inputs from the TRN.
- Mice in the CSD experimental group showed lower levels of N-arachidonoyl dopamine (NADA) in the TRN compared to control mice.
- In mice subjected to CSD, administration of NADA resulted in reduced sensitivity to pain, which was observed by higher mechanical withdrawal thresholds.
- NADA significantly reduced heightened neural activity in the VP, which was originally caused by CSD.
Activity of TRN and VP due to CSD and decreased levels of NADA
Although CSD has been shown to promote pain sensitivity, the underlying mechanisms had not been fully explored, until now. Shen’s team has demonstrated that not only does the TRN play a role in increasing pain sensitivity with regards to sleep deprivation, but it also projects to other brain regions, such as the VP, and those connections also play a role in the development of hyperalgesia. Increased activity of TRN and VP neurons both led to an increase in hyperalgesia in mice. Through their study, they identified that CSD also results in decreased levels of NADA, which contributes to hyperalgesia, but administration of NADA to mice that were deprived of sleep resulted in a reduced perception of pain.
Sleep deprivation can impact anyone, but it particularly affects those with sleep disorders, and this study has shown that a lack of sleep can lead to physiological changes that can increase pain perception. By understanding this, it may become more apparent to people why getting a good night’s worth of sleep is important. There is an underlying brain network, involving both the TRN and the VP, as well as neurotransmitters, such as NADA, that provide proof of this. Furthermore, the role of NADA in this network suggests potential for its use in developing therapeutics for heightened pain perception in individuals with chronic sleep disturbance.
Further experimentation is required to improve understanding of the role of NADA, the TRN and VP in pain sensitivity due to CSD. One limitation is the narrow scope of this research, as pain modulation has been shown to involve other brain regions too. There is therefore potential for other regions to be involved in hyperalgesia due to CSD as well. Furthermore, this research was done in a mouse model and CSD could demonstrate different neuronal-level changes in the human brain, so the results of this study may not be directly applicable to human research.
Drug development involving NADA
The next step of this research would be to explore NADA further to investigate the potential of developing it into a therapy that could first be tested in mice and then in clinical trials. This research has provided insight on the mechanisms underlying hyperalgesia due to CSD, but in order to use these results to generate a clinical impact, it would be beneficial to consider how this research could inform drug development.
Reference: Ding W, Yang L, Shi E, et al. The endocannabinoid N-arachidonoyl dopamine is critical for hyperalgesia induced by chronic sleep disruption [published correction appears in Nat Commun. 2023 13;14(1):7342]. Nat Commun. 2023;14(1):6696. doi:10.1038/s41467-023-42283-6