Harnessing the Power of the Immune System: Advances in Cancer Immunotherapy
Researchers have developed innovative treatment strategies by understanding the interactions between cancer cells and the immune system.
Complete the form below to unlock access to ALL audio articles.
Understanding the pivotal role of the immune system in cancer is revolutionizing treatment – and also offers tantalizing opportunities for disease prevention.
The immune system is most well-known for its critical role in identifying foreign pathogens, such as bacteria and viruses, and destroying them. But these defenses have also evolved to safeguard us from threats from within the body.
“The immune system has evolved to protect us against lethal infections,” explains Tim Elliott, Kidani professor of immuno-oncology at the University of Oxford. “But the same system also helps to protect us from cancer – by recognizing and eliminating rogue cells before they can cause harm.”
By understanding the interactions between cancer cells and the immune system, researchers have developed innovative treatment strategies. These novel approaches seek to either enhance the body’s natural defenses against cancer or remove the obstacles hindering immune cells from finding and destroying tumor cells.
“Immunotherapies are a significant addition to cancer’s therapeutic toolkit – and they’re here to stay,” says Dr. Astero Klampatsa, group leader in cancer immunotherapy at The Institute of Cancer Research, London. “In the future, I think immunotherapies will become more precise, more effective and establish themselves as a hallmark in cancer treatment.”
Researchers are striving to expand the reach of these revolutionary therapeutics to more cancer patients. They are also exploring exciting new opportunities to deploy them to prevent the disease from developing in the first place.
Immune surveillance
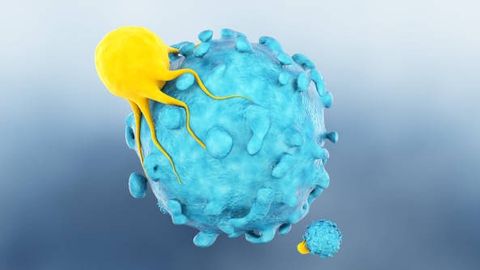
Immune cells (such as killer T cells) are constantly patrolling our bodies – detecting and destroying foreign pathogens, or precancerous or cancerous cells before they can develop into full-blown cancer.
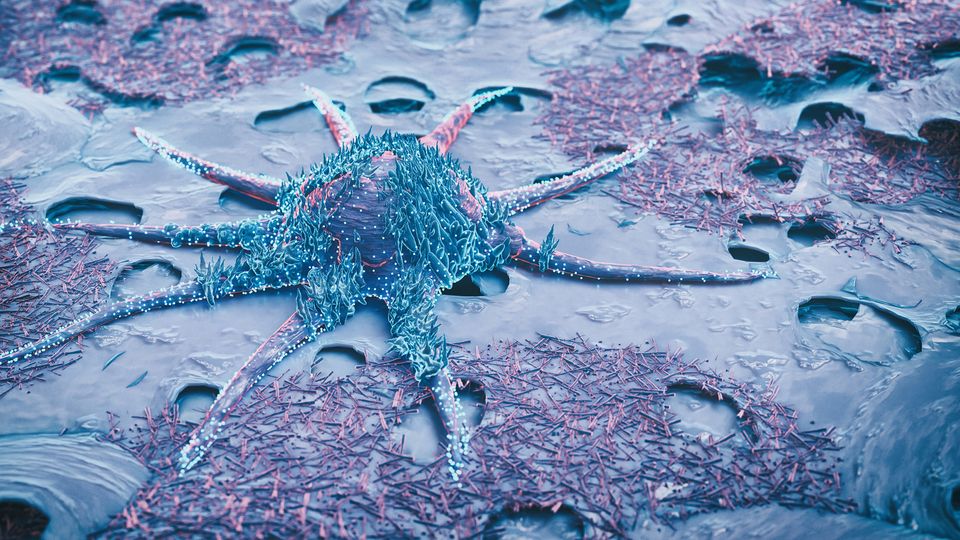
“Cancer arises when a cell loses the ability to listen to normal cues that tell it when to divide, when to stop dividing, and when to die,” explains Elliott. “When these circuits go wrong, it starts to divide out of control – and left unchecked, it can develop into a tumor.”
Immune cells recognize threats by surveilling proteins (or antigens) found on the surface of all cells in the body. This enables them to examine a potential threat closely and decide whether to attack. However, despite the remarkable capabilities of the immune system, cancer cells have evolved escape mechanisms.
“There are all sorts of sneaky and clever ways that tumors use to evade detection by the immune system,” says Elliott.
One strategy used by tumor cells is the downregulation or alteration of their surface antigens, making them less visible to the immune system. They can also manipulate the tumor microenvironment to their advantage – such as by blocking the entry of immune cells or by producing molecules that suppress their function.
Transforming treatment
The foundation of immunotherapy lies in finding ways to counteract the strategies that cancer cells use to evade immune surveillance – or to empower cancer-fighting immune cells, like T cells, to overcome these defense mechanisms.
A prominent example of this new type of cancer treatment is a group of drugs called immune checkpoint inhibitors. These immunotherapies, which work by releasing the “brakes” on immune cells so they can find and attack cancer cells, are now approved to treat a variety of types of cancer, including breast, bowel and lung cancers.
“The immune checkpoint inhibitors work incredibly well in some patients – and they are even curative in certain cancers that have previously been very hard to treat,” says Elliott.
But a huge challenge is that these drugs don’t work for everyone.
“For example, only about a third of mesothelioma patients will benefit from immune checkpoint inhibitors – and these drugs are expensive and have toxicities,” says Klampatsa.
Identifying biomarkers that can accurately predict which patients will respond will enable doctors to identify those who are most likely to benefit, sparing others from unnecessary treatment and its associated side effects.
In pursuit of precision immunotherapy, Klampatsa is using a variety of techniques to characterize immune cells in blood and tumor samples collected from mesothelioma patients before treatment – and then applying bioinformatics to look for biomarkers associated with clinical outcomes.
“The immune system can tell us stories about how a tumor is likely to behave in a given situation – and we can use these to predict what will happen next,” she explains.
Other types of immunotherapies, such as adoptive cell therapies, are designed to boost the ability of the immune system to target and kill cancer cells. The approach involves collecting the patient’s immune cells (usually T cells), which are then either multiplied or genetically engineered in the laboratory, before putting them back into the body.
“The most famous example is the chimeric antigen receptor (CAR) T-cell therapies,” says Klampatsa. “These have shown remarkable success in blood cancers like leukemia and lymphoma – with some patients in long-term remission following a single dose of CAR T cells.”
But CAR T-cell therapies haven’t yet been shown to work well in solid tumors that, according to Klampatsa, “form highly treatment-resistant tumor masses, a completely different setting to blood malignancies where single cancer cells are circulating around the body.”
Researchers, like Klampatsa, are striving to find ways to improve the ability of CAR T-cell therapies to penetrate inside solid tumors and ensure they can efficiently function within the immunosuppressive tumor microenvironment.
Preventing cancer
As our understanding of the role of the immune system in cancer continues to deepen, the possibility of developing preventative vaccines is also gaining traction.
“It’s a really exciting area,” enthuses Elliott. “At the moment, prevention is mainly focused on modifying lifestyle factors – but I can see a time where it’s possible to have a vaccine that can help protect us from developing cancer.”
For the past decade, Elliott’s research has focused on uncovering the molecular details of a pathway that plays a key role in processing and presenting cancer-associated antigens on the surface of tumor cells, marking them for immune destruction.
“We’ve now developed mathematical models that can predict which bits of those antigens are most likely to be recognized by the immune system – and even better, which bits will provoke an immune response that’s more likely to get rid of the cancer,” he says.
Elliott hopes this approach will help inform the design of better vaccines (such as those made from whole cancer cells, proteins, DNA or RNA) for treating cancer. But his long-term sights are set on cancer prevention.
“For example, we’re targeting a group of individuals who have been diagnosed with early-stage lung cancer through screening,” he says. “After they’ve had surgery to remove the cancer, they still have around a 30% risk of recurrence – and we want to be able to offer them a vaccine that can bring that down to 0.”
The road ahead
Cancer immunotherapy represents a new paradigm in cancer care. The approach is already transforming the lives of some patients – and holds immense promise for the future.
“When you have something to start with, it opens up numerous new avenues for how to move forward,” says Klampatsa. “It provides the opportunity to explore them further, exploit them, advance them, improve them – and adopt them.”
Combining immunotherapies with other treatments, such as chemotherapy, radiotherapy or targeted drugs, has also shown promising results in clinical trials. As these treatments all work in different ways, such combination strategies offer the potential to eliminate cancer permanently. Personalizing treatment based on a patient's unique genetic and immunological profile also offers the prospect of more targeted and effective immunotherapy.
“Immuno-oncology is a fast-moving discipline,” says Elliott. “The added bonus is it’s rapidly deployable, so we can see discoveries move rapidly from the lab into the clinic - and that’s really exciting.
About the interviewees:
Tim Elliott is the Kidani professor of immuno-oncology at the University of Oxford
and co-director of the Cancer Research UK Oxford Centre. His research
focuses on antigen presentation and T cell biology, and he has incorporated
discoveries in antigen processing, T cell regulation and immunodominance into
the development of new cancer immunotherapies.
Astero Klampatsa is a group leader in cancer immunotherapy at The Institute of Cancer
Research, London. Her research focuses on unraveling the cellular mechanisms
responsible for the lack of T cell immune response, identifying markers of
response to immunotherapy and developing new CAR T-cell therapies for thoracic
cancers, especially mesothelioma.